Parents and Caregivers Guide
What is Ependymoma?
Ependymoma is a tumor of the brain and spinal cord. Ependymoma is the third most common form of childhood brain and spine tumors. Ependymomas can occur at any age, but most often occur in young children and are often diagnosed at ages less than three. Ependymomas in young children frequently recur after treatment. The treatments are often debilitating leading to a lifetime of disability.
What Causes Ependymoma?
The cause of ependymoma is entirely unclear. The tumor is thought to arise from the ependymal cells of the brain which ultimately form the lining of the entire ventricular system of the brain which serves as a vessel through which the cerebrospinal fluid circulates. These tumors can occur in multiple locations throughout the brain including the spinal cord, the brainstem (infratentorial, the portion of the brain in the lower back of the head) and in the brain (supratentorial, the portion of the brain at the highest point of the head.) Although tumors found in these different locations have the same histological appearance (appearance under a microscope), recent research has indicated that the tumors in these three locations are both different biochemically and differ dramatically in their behavior and prognosis.
Possible causes of ependymoma range from viral infection, exposure to ionizing radiation, lack of multivitamin use, exposure to pesticides, radio frequency radiation, exposure to organic solvents and random chance. There is little research to support any particular causative factor largely due to the rarity of the condition.
A recent 2019 study published in Nature, suggests that posterior fossa A tumors may actually originate prenatally from immature progenitor cells of the brain and that the lack of differentiated cell types in this type of tumor suggests a possible differentiation block.
Incidence
Ependymomas are the third most common brain tumor in children and young people under the age of 18, accounting for around 10% of pediatric brain tumors and close to 2% of all pediatric cancers. Half of all childhood ependymomas arise in children younger than five years of age and around one third in children under three years. Pediatric ependymoma is a rare tumor with an estimated 200 cases reported in the United States per year.
Diagnosis
A typical presentation would be for a child to present to a physician's office or emergency department with vague neurological symptoms such as inappropriate falls or a change in eye movement. Symptoms in the early stages can be hard to differentiate from normal pediatric behavior frequently leading to a delay in diagnosis.
As the tumor grows pressure builds up in the head. This can lead to the following general brain tumor symptoms:
- Enlargement of the head (in infants)
- Persistent headache (especially in the morning)
- Recurrent vomiting
- Seizures
- Changes in vision
- Changes in appetite
- Sleepiness
- Cognitive difficulties (difficulties concentrating or remembering)
If a tumor is suspected, an MRI scan will be performed which can reveal the location and texture of the tumor.
What happens once the diagnosis is made?
Once the tumor has been identified, a Neurosurgeon will be consulted to determine if the tumor can be resected. Typically, surgery is recommended, followed by radiation therapy. The technology in the surgical domain has advanced dramatically over the past 20 years to the point that many of these tumors can be successfully resected. However, many of these technologies are only available at highly specialized centers. If possible, you may want to consider transfer to one of these hospitals.
What determines what happens?
In many ways, the treatment of ependymoma is really surgical and the degree of resection determines the outcome of therapy. Some of the types of ependymoma have no evidenced based pharmacological treatment, so extra consideration before surgical resection is mandatory. Surgery can yield three possible outcomes. The first is gross total resection in which no residual tumor can be seen on a post operative MRI scan. Near total resection which < 5 mm of residual tumor can be seen on follow up examination. The final possibly is incomplete resection which may require a second surgery; sometimes recommended shortly after the first surgery. Another major pitfall with surgery is movement of the brain structures into the empty space left over after the resection of the tumor. This mass effect complicates assessment of images after resection. Follow up scans are also quite difficult to assess as the contrast agent used, gadolinium, can enhance tumor as well as other non-tumor tissues such as scar tissue and inflammation. This can lead to diagnostic confusion after the initial resection is completed and considerable experience and judgement is needed by a multi-disciplinary team including Neurooncologists, Neurosurgeons, Radiation Oncologists and Radiologists to determine the course of therapy.
What happens after the surgery?
The surgeries to resect ependymoma can be quite long and stretch out to 6-9 hours, which can lead to some tense moments for parents. In recovery, your child may have a variety of neurological defects including inability to walk or swallow or speak. The first 48 hours after surgery will be emotionally demanding. Much of this is related to the surgical process itself and many of these symptoms will clear during the recovery period from the surgery as the swelling from the tumor resolves after resection. Some of the defects, however, may persist and there can be permanent damage to neurological structures caused by the resection that are unavoidable due to the paramount need to remove all of the tumor that is possible.
Also complicating the post-operative course is pain related to the incision in the back of the head. In young patients, pain control is especially challenging as potent pain medications such as narcotics may complicate ongoing neurological assessments which are mandatory after brain surgery versus the use of less effective pain medications such as tylenol which may provide less effective pain control. If at all possible, tylenol should be given as a scheduled medication and not as needed to maximize the benefit of the medication without sedating the young patient.
Lastly, temporary placement of a feeding tube may be mandatory but is usually temporary and should not be viewed as a failure of the surgery. It is important for healing for the child to maintain body weight if at all possible.
In the few days after the surgery, there will be additional MRI scan(s) to assess the size of the ventricles (cerebrospinal fluid filled spaces) of the brain to determine if they are enlarged. If they are enlarged, it may indicate obstruction of the ventricular system by debris from the surgery. A temporary drain may need to be placed in the brain to allow time for the brain to clear the debris. The drain can be uncomfortable for the child, but you can manage some mobility with the drain in place with careful direction from the medical team taking care of your child.
How long does hospitalization last?
Generally, a hospitalization after resection of ependymoma will last 1-2 weeks depending on the difficulties encountered after surgery. There may be a recommendation to go to rehabilitation, which should be considered. Upon return home, there will likely be some regression in behavioral habits over the 8 weeks following surgery and the parents will need to be mentally prepared for that.
What happens with radiation?
Many patients with ependymoma will require radiation as well and placement of a drug port as small children generally require sedation to complete the radiation treatments. Radiation side effects vary greatly by child. Possible side effects include nausea, vomiting, dizziness, loss of appetite, hair loss, fatigue.
Support for families
As a family faces this diagnosis, they may require additional support. Your local hospital is a good place to begin to find support groups, and trained counselors. In addition, there is online support and community available through the following Facebook groups:
- Ependyparents: https://www.facebook.com/groups/ependyparents/
- Pediatric Ependymoma Parents Group: https://www.facebook.com/groups/374373836261746/
Information on prognosis
Due to the variability in location of the tumor and in the quality of the resection, long term outcomes with this tumor are difficult to predict. However, with current techniques, many young patients will be able to return a good functional status and continue their personal development. Research studies regarding long term outcome have yielded variable results and many reflect changes in treatment patterns over time.
Prognosis Varies with Individual
Determining the individual prognosis of a patient with ependymoma depends on many factors. Because the word ependymoma refers to a histological definition of the tumor, it lumps many different tumors which have unique physiologies together. Recent research has indicated that the classification of ependymoma has multiple subtypes depending on location of the tumor and the presence of a variety of many histological and genetic markers. More recently, some differentiation of the tumor types has been made based on the variable epigenetic landscape of the tumor whereby the differential expression of genes and not specific genetic mutations determine the behavior of the tumor. More recently, there has been discussion of another technique called DNA methylation profiling to examine patterns of methylation which determine which genes are turned off and on compared to normal tissues.
One trend that appears to pervade the literature regarding ependymoma is that the extent of resection after surgery is perhaps the strongest factor driving how a patient fares long term. Thus, a patient with a tumor that is in a location which is easier to resect (such is in the midline of the brain) will generally fare better than one with a tumor in a more challenging location.
Available Now!
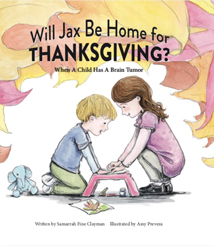 All profits from the purchase of the book will be directed to pediatric brain tumor research.
All profits from the purchase of the book will be directed to pediatric brain tumor research.